EPCON Highlights Data-Driven TB Hotspot Mapping at The Union Conference in Copenhagen
- Dec 3, 2025
- 2 min read
At this year’s Union World Conference on Lung Health in Copenhagen, our Data scientist Lead Anne-Laure Budts had the opportunity to share two of our latest explorations into predictive modelling for tuberculosis (TB).
One focused on Uganda, the other on the Philippines — two countries with very different landscapes, data environments and health systems. Yet both showed the same powerful truth: when routine TB screening data is combined with geospatial context and the right modelling techniques, the data begins to reveal patterns that can fundamentally reshape how countries find and respond to TB.

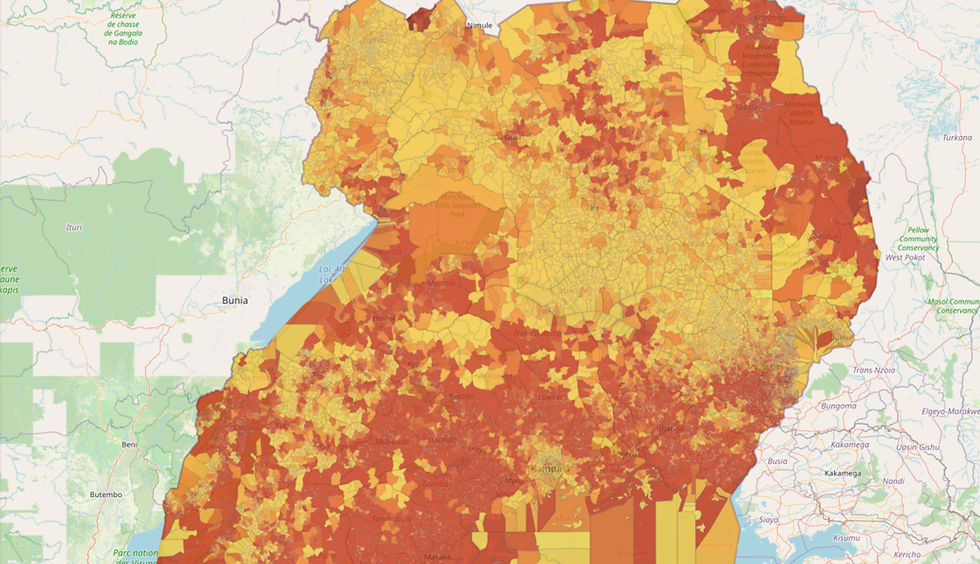
Uganda: From 10,000 Spatial Clusters to Clearer Hotspots
In Uganda, we set out to understand TB risk through a more spatially sensitive lens. To do that, we combined retrospective Active Case Finding (ACF) data with demographic, environmental and socioeconomic indicators — everything from travel time to the nearest health facility to patterns of malnutrition and deprivation.
Using weighted k-means, we divided the country into 10.000 meaningful spatial clusters, each capturing a blend of TB outcomes and local context. We then tested several modelling approaches using district-level cross-validation to challenge the models with data from completely unseen areas.
What stood out was the performance of Naive Bayes, which identified TB hotspots with a 44% higher relative risk in the top predicted areas. Fast and surprisingly powerful, the model proved that sometimes the most effective solution is the one most closely aligned to the structure of the data.
Today, the Uganda model is fully integrated into the Epi-control platform, where health teams can explore hotspot predictions, visualize trends and plan targeted ACF strategies.
Philippines: High-Resolution Prediction at Barangay Level
In the Philippines, the challenge - and opportunity - was different. With nearly 42.000 barangays, each with unique environmental, social and accessibility characteristics, the model needed to operate at a far more granular scale.
We brought together ACF outcomes with indicators such as water access, nightlight intensity, female literacy, road networks and self-organizing map encodings of population and land type. Then, using province-level cross-validation, we asked the same question:
Which model best captures risk in completely unseen regions?
Again, Naive Bayes came out on top, identifying bacteriologically confirmed TB hotspots with a 48% higher relative risk, and performing even better when predicting all-forms TB. The clarity and stability of these predictions reinforced how well Bayesian models match the structure of barangay-level data.
The Philippine model is now embedded in the Epi-control platform, offering real-time hotspot detection and helping health workers prioritize barangays with greater precision.
Conclusion
Despite the differences between Uganda and the Philippines, a common thread runs through both projects: the best model is the one that fits the context. In both cases, Bayesian approaches delivered the strongest and most reliable predictions - because they are well suited to the patterns and distributions within the data.
For EPCON, these findings reaffirm our purpose: turning routine health data into practical, actionable insights that help health systems detect TB earlier, deploy their resources more effectively and reach vulnerable communities faster.
We’re excited to continue this work across more countries — and to keep following where the data leads next.